Updated March 2022
Questions about the COVID-19 virus or the vaccines to combat it? Read here for current research and updates from our authors and educational partners as well as scientists and science writers.
Information about COVID-19
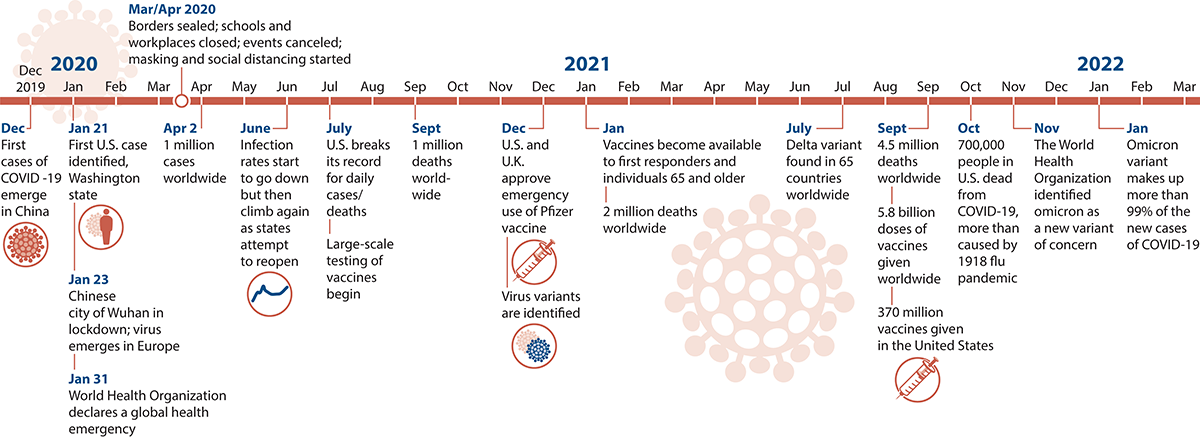
Since December 2019, discussion of COVID-19 has dominated the news and social media. Here are some of the significant moments in the pandemic.
What Is a Virus?
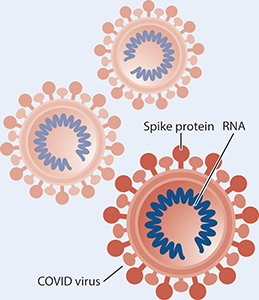
A virus is a small, infectious particle that consists of genetic material (RNA, in the case of the virus that causes COVID-19) and an outer coating that protects the genetic material. Viruses can only live and multiply inside a host, which is a living organism such as a human, animal, or plant. Viruses, like other microbes, have been on Earth for billions of years.
We coexist peacefully with most microbes, and some (like the bacteria in our gut) actually help us. But throughout human history, some pathogens have caused worldwide illness (pandemics).
What Is COVID-19?
COVID-19 is a disease caused by a type of virus called a coronavirus. Viruses cause many diseases, including the common cold, flu, and HIV. Each viral disease is caused by a unique virus with unique features. The COVID-19 virus is covered with proteins in the shape of spikes, like a jeweled crown (corona is Latin for crown).
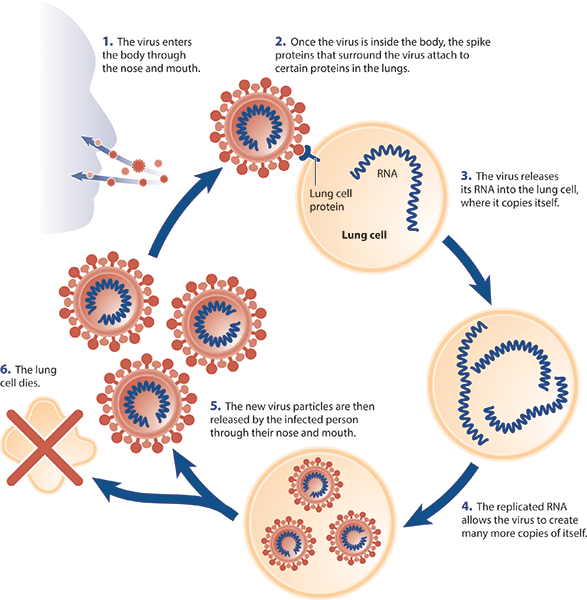
The COVID-19 virus enters our bodies through our noses and mouths, and then uses its spike proteins to enter cells in our respiratory tracts. Once inside human cells, the virus uses its own genetic material to replicate itself. Eventually, the virus replicates itself sufficiently so that those infected cells start releasing the virus back out into the world, again through our noses and mouths. That is when we become contagious, spreading the virus to other people.
As our immune systems work to battle the invading virus, we develop the symptoms of the illness, including fever, body aches, and dry cough. Fortunately, most of us have an immune system that is strong enough to win the battle, even though it may take weeks or even months to recover. Unfortunately, many people lose the battle. Worldwide, about 5.7 million people have died from COVID-19 as of January 2022. Nearly 900,000 had died in the United States by early February 2022.
The longer viruses are present in our environment, the more likely they are to mutate and form a new strain or variant. We first saw the delta variant, which was more contagious than the original strain of COVID-19. In late November, the World Health Organization identified another variant of concern: the omicron variant, which is even more contagious but may cause less severe infection. Omicron now represents almost all of the COVID-19 infections being identified.
What Role Does Evolution Play in the COVID Pandemic?
COVID-19 is a case study in evolution. Virologists have been able to observe evolution in action in weeks or even days during the progression of the COVID pandemic. As Pulitzer Prize winning New York Times journalist and Macmillan Learning coauthor of Evolution: Making Sense of Life Carl Zimmer explains in this podcast, mutations in the virus are the fuel for evolutionary change.
How Do I Know If I Have COVID-19, a Cold, or the Flu Based on My Symptoms?
Many of the symptoms of each illness are similar, and some symptoms can even resemble allergies. The Mayo Clinic has developed symptom comparison tables that may help you determine whether you are likely to have COVID-19, a cold, the flu, or are experiencing allergies. However, the only way to be confident about the cause of your symptoms is to get tested.
How Does COVID-19 Move Through the Environment?
The virus that causes COVID-19 is an airborne virus. This means that it can only travel and reproduce by passing through the respiratory system of mammals like us. The ability for an airborne virus to be infectious depends a lot on the environment. For example, the virus is less concentrated in outdoor and well-ventilated indoor spaces, which reduces its ability to move from one host to another. See this video for an example of how a virus can spread through the air in various environments. (Note that this video recommends keeping a distance of 1 meter, whereas current recommendations call for a distance of 6 feet.)
Should I Worry about Spreading COVID-19?
Before the coronavirus pandemic, did you ever go into work even if you felt a little sniffly? A few days later, one of your co-workers would start showing the same symptoms. A few days after that, a few more people would catch it. “There’s a cold going around,” everyone would say, just part of the world of work. We’d all shrug it off.
Still, back then, even before we were masking and social distancing, we knew that some illnesses were more contagious and more dangerous than others. You might come to work with a cold, but you wouldn’t come to work with the flu, or measles, or chickenpox, because more people would get sick—and some would get seriously sick.
So how contagious is the COVID-19 virus? This graphic and information from the Centers for Disease Control and Prevention shows that if you are an unvaccinated person infected with COVID-19, you are likely to spread it to many other people—even if you don’t know you’re infected. The omircon variant is a lot more contagious than the flu and almost as contagious as chickenpox.
How many people you spread it to is known as the virus’s reproductive number, or R0. The omicron variant’s high R0 is causing the pandemic to spread exponentially. Exponential growth means the virus can spread incredibly quickly.
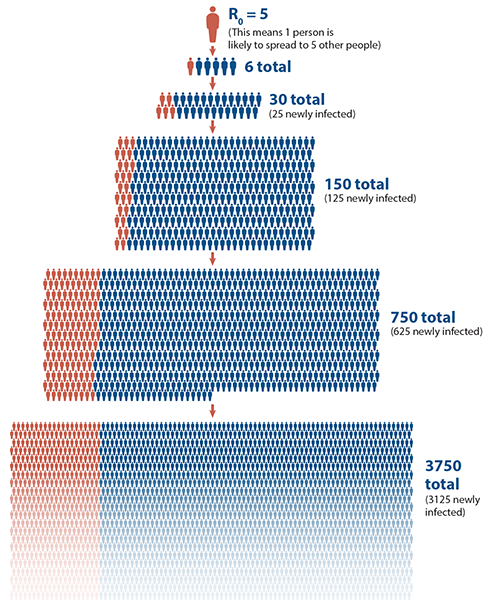
This figure shows how infection spreads using a value of R0 = 5, which means one person is likely to infect another five.
(Newly infected individuals are represented with blue icons. Previously infected individuals are represented with red icons.)
So Far, I'm Good. What Are the Chances I Will Catch COVID-19?
If you have managed to avoid getting sick so far in the pandemic, you may feel that the worst is over. Unfortunately, the current surge and the appearance of new variants like omicron indicates that until most of the world’s population is vaccinated, the number of cases will remain high and hospitals will continue to fill with seriously ill patients.
It’s now clear that anyone—vaccinated or unvaccinated—can transmit the disease, although people who are vaccinated are less likely to spread COVID-19 and less likely to become seriously ill. You can reduce your risk by being fully vaccinated—meaning initial vaccines and a booster shot, wearing a mask, social distancing, and avoiding indoor gatherings.
Some areas have been harder hit than others. Are you curious about how widespread COVID-19 is in your area? You can estimate the chance that at least one COVID-19-positive person will be at an event or venue you visit using the COVID-19 Event Risk Assessment Planning Tool. Created by scientists at Georgia Tech, Duke, and Stanford universities, this tool lets you calculate how risky an event may be by adjusting the number of people attending.
You can access statistics about infection rates and deaths by country and see how case numbers are changing daily or monthly at the COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University.
If I've Already Had COVID-19, Am I Immune to It?
No. Unfortunately, individuals who have had COVID-19 and recovered can get reinfected. In this study reported by the CDC, individuals who were not vaccinated were more than twice as likely to be reinfected compared with those with full vaccination.
How Has COVID Changed the World?
Accelerated development of cutting-edge PCR tests, advances in messenger RNA therapies, an increasingly overburdened healthcare system, growing global inequality, and long-term changes in our work life are just some of the examples of how COVID has changed our world forever. See the special issue of Scientific American for more.
What Should I Know About Long COVID?
Some people infected with the COVID-19 virus may develop what is commonly referred to as long COVID. These people experience a variety of symptoms, including shortness of breath, fatigue, and difficulty with thinking and concentration–often described as brain fog–a month or more after they are initially infected. Anyone can develop long COVID, even if the initial infection had few or no symptoms.
Although not much is known about what makes some individuals more or less likely to develop long COVID, recent research has suggested that long COVID is more likely to occur in people with a number of coexisting conditions. Researchers are currently working to understand how long COVID affects the body, and how it might be treated. In the meantime, the best way to avoid long COVID is to get vaccinated and boosted against the COVID-19 virus and prevent the initial infection.
